Introduction: Primary mediastinal B cell lymphoma (PMBL) is clinically and biologically distinct from the other subtypes of diffuse large B cell lymphoma (DLBCL), typically affecting young female patients (pts) with a bulky mediastinal mass. Standard treatment (TRT) is a combination of anti-CD20 antibody (Ab) and anthracycline-based chemotherapy. We aimed to compare patients' outcomes after CHOP delivered every 21 days (CHOP21) or 14 days (CHOP14) or ACVBP combined with anti-CD20 Ab in real life.
Methods: All Pts treated in LYSA centers were eligible in this retrospective analysis. Inclusion criteria were as follow: age ≥18 years (yrs), newly diagnosed PMBL, TRT with CHOP or ACVBP plus anti-CD20 Ab between 2006 and 2017, and patient non-opposition statement. Primary endpoint was progression-free survival (PFS), secondary endpoints were: overall survival (OS), response rate (Lugano 2014) and total metabolic tumor volume (TMTV).
Results: 313 pts were enrolled from 25 LYSA centers in France and Belgium. In all, median age at diagnosis was 32 (18-88) yrs. Majority of pts were female pts (60.7%) and presented at diagnosis with a good performance status (0-1: 81.8%), stage I-II (57.5%), elevated LDH (85%), Bulk>10cm (58.5%) and low/low-intermediate aaIPI 0-1 (56.7%). Pts in the CHOP21 (n=57) group were older (median 40 yrs, vs 33 vs 29.5, p<0.001), had more frequent low/low-intermediate risk aaIPI (71.4%, vs 55.6% vs 52.5%, p=0.044) and displayed a lower proportion of elevated LDH (66.7%, vs 88.2% vs 83.9%, p=0.014) as compared to CHOP14 (n=76) and ACVBP (n=180), plus anti CD20 Ab (Rituximab: n=296, obinutuzumab: n=17). 229 pts (73.2%) received intrathecal prophylaxis. Median number of chemotherapy cycles for CHOP21, CHOP14 and ACVBP groups were: 6 (1-8), 7.5 (1-8) and 4 (1-4), respectively. Consolidation ASCT was performed for 1 (1.8%), 24 (31.6%) and 46 (25.6%) pts, (p<0.001) and mediastinal RT was delivered to 2 (3.5%), 11 (14.5%) and 4 (2.2%) pts, respectively (p<0.001). ASCT + RT was done for 0, 5 (6.6%) and 3 (1.7%) pts, respectively (p=0.043). Baseline TMTV assessment was available for 233 pts (74.4%).
Complete metabolic response rates at end of TRT were comparable between CHOP21, CHOP14 and ACVBP groups: 81.1%, 90.9%, and 85.5%, respectively (p=0.46).
37 (11.8%) pts progressed including 32 (10.2%) who displayed primary refractory disease and 6 (16.2%) pts who relapsed after consolidation ASCT. CNS relapse occurred in 9 (2.9%) pts. Median time between ASCT and relapse was 3 (2-58) months. Patients received the following salvage TRTs: high dose chemotherapy (HDC: R-ICE/R-DHAOX-like) (n=30) followed by second-line consolidation ASCT (n=11/30) and post-ASCT mediastinal RT (n=5/11); salvage RT without chemotherapy (n=1); other regimens (R-CHOP, R-GEMOX) (n=3); none (n=3). 2-yrs second PFS (PFS2) rates in pts who had previously received CHOP21, CHOP14 and ACVBP were: 20.5% vs 62.5% vs 18.8% (p=0.43). Only HDC + ASCT strategy granted disease control (2-yrs PFS2: 32.3%).
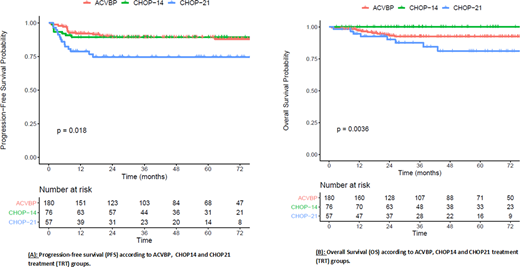
Median follow up was 44 (1-153) months and the CHOP21, CHOP14, ACVBP 5-yrs PFS and 5-yrs OS were: 74.7% (95%CI: 64-97.1%), 89.4% (82.7-96.6%), 89.4% (84.8-94.2%) (p=0.018, Figure A); and 81% (70-94.4%), 100% (100-100%), 92.4% (88.4-96.7%) (p=0.0036, Figure B), respectively. In a multivariate model including TRT group, consolidation ASCT and/or RT, aaIPI, Bulk>10cm and TMTV≥360cm3, CHOP14 was not associated with better PFS as compared to ACVBP and CHOP21 (p=0.1548). Baseline higher TMTV (≥ 360 cm3) was associated with lower PFS in multivariate analysis, independently of TRT (HR=0.41 [0.2-0.85], p=0.02).
All grades TRT-related adverse events were similar between the groups, except for an excess of febrile neutropenia (5.3% vs 5.3% vs 24.4%, p<0.001) and mucositis (1.8% vs 3.9% vs 22.8%, p<0.001) in the ACVBP group. Twenty-two pts died (CHOP21: n=8, ACVBP: n=14) mainly due to lymphoma progression (n=15; 68.2%). 2 toxic deaths were observed (CHOP21: n=1, ACVBP: n=1). Secondary malignancies appeared in 7 pts (CHOP21: n=2, ACVBP: n=5), including 3 cases of acute myeloid leukemia.
Conclusion
These results confirm the favorable outcome of PMBL pts treated with CHOP14 and ACVBP plus anti CD20 Ab. The toxicity of ACVBP was more pronounced and CHOP14 was associated with a better OS. Baseline TMTV≥360cm3 is a highly predictive factor of unfavorable outcome in PMBL pts, independently of TRT. We recommend R-CHOP14 as standard of care in PMBL.
Camus:ROCHE: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company); PFIZER: Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company); AMGEN: Honoraria; JANSSEN: Honoraria. Decazes:Bayer: Other: travel, accomodations, expenses. Bernard:Janssen: Other: Travel and accommodation . Gandhi Laurent:Abbevie, Pfizer, Takeda, Roche: Other: Travel; Roche, Takeda, Iqone, Accord: Consultancy; Roche, Takeda, Accord: Honoraria. Laribi:amgen: Research Funding; novartis: Honoraria, Research Funding; takeda: Research Funding; abbvie: Honoraria, Research Funding. Houot:Gilead: Honoraria; Kite: Honoraria; Roche: Honoraria; Novartis: Honoraria; Janssen: Honoraria; Celgene: Honoraria; Bristol-Myers Squibb: Honoraria; MSD: Honoraria. Tilly:BMS: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal